High Oxalate Foods and Kidney Stones

The discomfort of passing a kidney stone has often been described as being as painful as childbirth. Ouch! For anyone who’s experienced this, your healthcare provider may have advised a low-oxalate diet to prevent you from developing kidney stones again.
Oxalates (or oxalic acids) are compounds in plant-based foods, including leafy green vegetables (kale, collard and mustard greens, spinach), beans, lentils, nuts, and seeds. While these foods are nutritious and safe for most people, you may need to limit them while following a low-oxalate diet. Oxalate is also made naturally in our bodies.
Your kidneys normally process oxalate from foods, and it’s removed in urine. If too much oxalate is consumed or produced, it may attach to minerals (like calcium), causing stones or crystals to form. Calcium oxalate stones are the most common type of kidney stones. [1] Bargagli M, Tio MC, Waikar SS, Ferraro PM. Dietary Oxalate Intake and Kidney Outcomes. Nutrients. 2020 Sep 2;12(9):2673. doi: 10.3390/nu12092673. PMID: 32887293; PMCID: PMC7551439.
As mentioned above, green leafy vegetables like spinach contain oxalate. A few other high-oxalate foods include rhubarb, almonds, beets, and sweet potatoes. Fortunately, you can still eat these foods in moderation, and there are ways to reduce your oxalate intake.
This review provides sound research and expert nutrition advice for individuals needing to follow a low-oxalate diet. We’ll offer tips and tricks to reduce oxalate in your diet while still enjoying the foods you love.
What Are Oxalates?
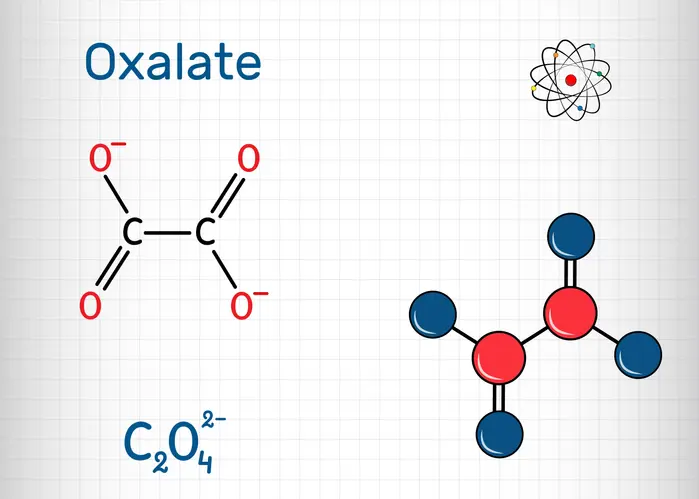
Oxalates are compounds found naturally in several plant foods. The most common foods containing oxalates are spinach, nuts and seeds, and some beans. Other foods like raspberries and figs may also contain small amounts of oxalates.
Oxalates have important roles for plants. They help manage and regulate their mineral content and protect the plant from damage from insects and other pests. Oxalates are necessary for the plants’ survival.
If the metabolism and excretion of oxalates are disrupted, oxalate can combine with minerals such as calcium and create crystals in the urine. When this happens, these crystallized compounds are hard to pass and may cause UTIs (urinary tract infections) and other problems. [2] Shen C, Zhu Q, Dong F, Wang W, Fan B, Li K, Chen J, Hu S, He Z, Li X. Identifying Two Novel Clusters in Calcium Oxalate Stones With Urinary Tract Infection Using 16S rDNA Sequencing. Front Cell Infect Microbiol. 2021 Nov 17;11:723781. doi: 10.3389/fcimb.2021.723781. PMID: 34869053; PMCID: PMC8635737.
Thankfully, not everyone has to avoid oxalates in their diet. Some individuals have a rare genetic condition called primary hyperoxaluria (PH). Their liver produces excess oxalate. If you have this condition or a history of calcium oxalate kidney stones, it may be necessary to follow a low-oxalate diet. [3] Michael M, Harvey E, Milliner DS, Frishberg Y, Sas DJ, Calle J, Copelovitch L, Penniston KL, Saland J, Somers MJG, Baum MA. Diagnosis and management of primary hyperoxalurias: best practices. Pediatr Nephrol. 2024 Nov;39(11):3143-3155. doi: 10.1007/s00467-024-06328-2. Epub 2024 May 16. PMID: 38753085.
Melissa Altman-Traub MS, RDN, LDN, notes, “According to the National Kidney Foundation, consuming foods high in calcium with foods that contain oxalate can bind to the oxalate and decrease the chance for kidney stones to form.”
She suggests substituting high-oxalate foods (such as raspberries) with low-oxalate foods, like blueberries.
Who Should Limit High Oxalate Foods?
Individuals with a history of calcium oxalate kidney stones
As mentioned above, individuals with a history of calcium oxalate stones are advised to limit how much oxalate they consume in their diets. This helps to reduce the amount of oxalate that could bind with calcium or other minerals to form painful crystals.
Those with malabsorption syndromes
Calcium oxalate stones may be more common in individuals with malabsorption conditions such as Crohn’s disease, pancreatitis, and bariatric surgery. When fat isn’t absorbed, increased free fatty acids are available to bind to calcium.
This leads to an increased amount of unbound oxalate absorbed in the large bowel. It then goes to the kidneys and can cause damage. Malabsorption conditions can also lead to fluid loss, increasing the risk of dehydration and kidney stones.
Malabsorption of nutrients such as calcium also makes it more difficult for the body to get rid of oxalate. In bariatric surgery, it may be due to increased absorption of oxalate in the colon, resulting in hyperoxaluria. [4] Bhatti UH, Duffy AJ, Roberts KE, Shariff AH. Nephrolithiasis after bariatric surgery: A review of pathophysiologic mechanisms and procedural risk. Int J Surg. 2016 Dec;36(Pt D):618-623. doi: 10.1016/j.ijsu.2016.11.025. Epub 2016 Nov 12. PMID: 27847289.
People advised by doctors to follow a low-oxalate diet
A low-oxalate diet is a specific diet that a medical professional would prescribe for those who need it. It isn’t a “fad diet” that would be followed for any other reason than to prevent or treat kidney stones. This type of diet isn’t necessary unless advised by a doctor.
Others typically do not need to worry unless advised
As several plant-based foods are nutritious but may have higher levels of oxalates, keep these foods in your diet unless otherwise indicated. Ignore the nutrition noise on the internet that oxalates are “anti-nutrients” because they bind minerals. [5] 10 Antinutrients to Get Out of Your Diet Immediately - Dr. Axe
Another misconception called “oxalate dumping” suggests that oxalate gets stored in our bodies and is only flushed once we remove it from our diets. [6] A List of 112 Foods High In Oxalate (Oxalic Acid) - Nutrition Advance
List of 25+ Foods High in Oxalates
Foods are categorized from very high oxalate to low oxalate accordingly: very high oxalate: 300 mg or more per serving, high oxalate: 100-299 mg per serving, moderate oxalate: 25-99 mg per serving, low oxalate, under 25 mg per serving. [7] Oxalate-List-1
Most people naturally eliminate oxalate through normal digestion. Harvard has a comprehensive list of oxalate content in food. [8] Harvard-Oxalate-Food-List-v2.3.1.pdf
Vegetables
1. Spinach - Very High

While spinach is very high in oxalate, boiling it will reduce its oxalate content. [9] Chai W, Liebman M. Effect of different cooking methods on vegetable oxalate content. J Agric Food Chem. 2005 Apr 20;53(8):3027-30. doi: 10.1021/jf048128d. PMID: 15826055.
2. Beets - High
Enjoy a small serving of beets to reduce your oxalate intake.
3. Swiss chard (Red or Green) - Very High
Like spinach, cooking Swiss chard reduces its oxalate content.
4. Rhubarb - Very High
Rhubarb isn’t commonly eaten, so you may not miss this in your diet.
5. Okra - Very High
Okra, like rhubarb, is an acquired taste. Unless you eat gumbo often, it’s likely not a problem. If needed, substitute bell peppers for okra.
Fruits
Fruit can also be a source of oxalates in your diet.
6. Figs - Moderate
Eat fewer figs to reduce your oxalate intake.
7. Kiwi - Moderate
Choose tangerines instead.
8. Raspberries - Moderate
Cut the serving in half to reduce oxalate intake.
9. Blackberries - Moderate
Swap blackberries with blueberries, which are lower in oxalate.
10. Concord grapes - Moderate

Choose green grapes instead of concord grapes
Nuts & Seeds
Nuts and seeds have varying amounts of oxalate. By substituting different nuts, you can reduce your oxalate intake.
11. Almonds - High
Swap almonds with pistachios.
12. Cashews - High
Enjoy pistachios instead of cashews.
13. Peanuts - High
Choose walnuts in place of peanuts for less oxalate.
14. Chia seeds - Very High
Use ground flaxseed instead.
15. Sunflower seeds - moderate
Substitute pumpkin seeds.
Grains & Legumes
16. Buckwheat - High
Use chickpea flour, which is also gluten-free.
17. Soybeans - Moderate
Try lentils instead.
18. Great Northern or Navy beans - Moderate
Substitute kidney beans.
19. Brown, long grain or wild rice - Moderate
Use white rice instead.
20. Whole wheat products - Moderate
Choose enriched wheat products.
Beverages
21. Black tea - Moderate
Enjoy green tea in place of black.
22. Hot chocolate - Moderate
Use milk chocolate versus dark chocolate, which is higher in oxalate.
23. Soy milk - Moderate
Try oat milk as a plant-based alternative to soy milk.
Other Foods
24. Cocoa powder - Moderate
Use milk cocoa when available.
25. Tofu - Moderate
Soft tofu is lower in oxalate than firm tofu.
26. Sweet potatoes - Moderate

Substitute turnips for sweet potatoes.
How Much Oxalate is Too Much?
For the general public who don’t need to avoid oxalate, no “safe” upper limit has been established. Most people digest and eliminate oxalate without issues and should consume plant-based foods for overall health. [10] Petroski W, Minich DM. Is There Such a Thing as "Anti-Nutrients"? A Narrative Review of Perceived Problematic Plant Compounds. Nutrients. 2020 Sep 24;12(10):2929. doi: 10.3390/nu12102929. PMID: 32987890; PMCID: PMC7600777.
For those who need to follow a low-oxalate diet to prevent kidney stones, health professionals advise between 50 to 100 mg of oxalate per day.
Bioavailability refers to the absorption of nutrients and other compounds. The bioavailability of oxalates isn’t consistent, so not all oxalates consumed will be absorbed in the body.
To prevent kidney stones, it’s important to obtain enough calcium in your diet. Calcium attaches to oxalate to help your body get rid of it safely. A low-calcium diet is a risk factor for the development of kidney stones. [11] Calcium oxalate stone - Causes, prevention, treatment | National Kidney Foundation
Tips to Reduce Oxalate Absorption
Pair high-oxalate foods with calcium-rich foods
Jessica (Clancy) Strawn MA, RDN a dietitian and expert in kidney disease from Houston, suggests food pairing. “Research shows that consuming calcium- and potassium-rich foods can help block the absorption of oxalates in the intestines, reducing the risk of kidney stone formation.” [12] Betz, Melanie. Whole Diet Approach to Calcium Oxalate Kidney Stone Prevention, Journal of Renal Nutrition, Volume 32, Issue 1, 2022, Pages e11-e17, SSN 1051-2276, https://doi.org/10.1053/j.jrn.2021.10.005.
Drink plenty of water
Staying hydrated helps prevent kidney stones. Water helps your kidneys excrete oxalate to prevent it from binding to other minerals and forming crystals.
Boil vegetables like spinach
As mentioned earlier, boiling spinach will decrease its oxalate content. Discard the water used for boiling and don’t use for soup or stew.
Avoid high doses of vitamin C
Vitamin C supplements taken in high doses pose a risk for kidney stones, as vitamin C can convert to oxalate. If you use vitamin C, avoid taking more than 1000 mg per day. [13] Doseděl M, Jirkovský E, Macáková K, Krčmová LK, Javorská L, Pourová J, Mercolini L, Remião F, Nováková L, Mladěnka P, On Behalf Of The Oemonom. Vitamin C-Sources, Physiological Role, Kinetics, Deficiency, Use, Toxicity, and Determination. Nutrients. 2021 Feb 13;13(2):615. doi: 10.3390/nu13020615. PMID: 33668681; PMCID: PMC7918462.
Limit intake of multiple high-oxalate foods in one meal
To prevent consuming too much oxalate, limit the intake of foods high in oxalate in one meal. There are plenty of low-oxalate foods to choose from.
Should You Avoid All Oxalate Foods?
- No. Many high-oxalate foods are also rich in nutrients, fiber, and antioxidants.
Several plant-based foods may be high in oxalates. However, a plant-based diet is also a source of important nutrients, including fiber, vitamins, minerals, and antioxidants. These foods help prevent disease and should be included in your diet. [14] Craig WJ, Mangels AR, Fresán U, Marsh K, Miles FL, Saunders AV, Haddad EH, Heskey CE, Johnston P, Larson-Meyer E, Orlich M. The Safe and Effective Use of Plant-Based Diets with Guidelines for Health Professionals. Nutrients. 2021 Nov 19;13(11):4144. doi: 10.3390/nu13114144. PMID: 34836399; PMCID: PMC8623061
Removing all foods containing oxalates is bad advice. These foods contain important nutrients, and when avoided, may lead to nutritional deficiencies
The goal of limiting oxalate in your diet is to enjoy those foods in moderation and strategically pair foods containing calcium with high-oxalate foods. One example would be pairing yogurt with raspberries or spinach with cheese.
If you need help planning meals, consult with a registered dietitian. A low-oxalate diet should only be prescribed by a medical professional. Dietitians can help you navigate it easier.
Sample Low-Oxalate Alternatives
- Swap spinach → romaine or kale
- Swap almonds → macadamia nuts
- Swap sweet potatoes → white potatoes
- Swap soy milk → dairy or almond milk (low-oxalate)
When to See a Doctor or Dietitian
After a kidney stone episode
A kidney stone shouldn’t be taken lightly. See your doctor if you suspect you’ve developed or are passing a kidney stone. They will guide you from there.
If advised to follow a low-oxalate diet
Seek the help of a registered dietitian if your doctor prescribes a low-oxalate diet. Information on the internet can be confusing and conflicting. Get information from a trusted source!
If confused about conflicting dietary info
If you’ve received conflicting nutrition information from your doctor or other healthcare provider, ask a dietitian to clear the confusion. We’re the food and nutrition experts.
For tailored, sustainable meal plans
Stacey Woodson, MS, RDN, LDN “Making dietary modifications can be challenging, especially when eating on the go. Therefore, I like to recommend low-oxalate foods that are readily available, such as broccoli, apples, and yogurt.”
Dietitians are available to offer sustainable, tailored meal plans for people needing low-oxalate diets.
Conclusion
Knowing which foods are high in oxalates is important, particularly for individuals with a medical history of kidney stones.
Staying hydrated and balancing your intake of high-oxalate foods is more effective than completely eliminating high-oxalate foods. Pair them with foods high in calcium to help your body eliminate oxalate.
Before making any significant diet changes, always consult with your medical provider first. If a low-oxalate diet is necessary, a dietitian is your go-to professional to help with the transition.
Was this article helpful?
-
Dietary Oxalate Intake and Kidney Outcomes. Nutrients. 2020 Sep 2;12(9):2673. doi: 10.3390/nu12092673. PMID: 32887293; PMCID: PMC7551439.; Bargagli M, Tio MC, Waikar SS, Ferraro PM. ;
https://pmc.ncbi.nlm.nih.gov/articles/PMC7551439/ -
Identifying Two Novel Clusters in Calcium Oxalate Stones With Urinary Tract Infection Using 16S rDNA Sequencing. Front Cell Infect Microbiol. 2021 Nov 17;11:723781. doi: 10.3389/fcimb.2021.723781. PMID: 34869053; PMCID: PMC8635737.; Shen C, Zhu Q, Dong F, Wang W, Fan B, Li K, Chen J, Hu S, He Z, Li X. ;
https://pubmed.ncbi.nlm.nih.gov/34869053/ -
Diagnosis and management of primary hyperoxalurias: best practices. Pediatr Nephrol. 2024 Nov;39(11):3143-3155. doi: 10.1007/s00467-024-06328-2. Epub 2024 May 16. PMID: 38753085.; Michael M, Harvey E, Milliner DS, Frishberg Y, Sas DJ, Calle J, Copelovitch L, Penniston KL, Saland J, Somers MJG, Baum MA. ;
https://pubmed.ncbi.nlm.nih.gov/38753085/ -
Nephrolithiasis after bariatric surgery: A review of pathophysiologic mechanisms and procedural risk. Int J Surg. 2016 Dec;36(Pt D):618-623. doi: 10.1016/j.ijsu.2016.11.025. Epub 2016 Nov 12. PMID: 27847289.; Bhatti UH, Duffy AJ, Roberts KE, Shariff AH. ;
https://pubmed.ncbi.nlm.nih.gov/27847289/ -
10 Antinutrients to Get Out of Your Diet Immediately - Dr. Axe;
https://draxe.com/nutrition/antinutrients/ -
A List of 112 Foods High In Oxalate (Oxalic Acid) - Nutrition Advance;
https://www.nutritionadvance.com/high-oxalate-foods/ -
Oxalate-List-1;
https://ohf.org/wp-content/uploads/2024/02/Oxalate-List-022724.pdf -
Harvard-Oxalate-Food-List-v2.3.1.pdf;
https://kidneystonediet.com/wp-content/uploads/sites/5/2024/05/Harvard-Oxalate-Food-List-v2.3.1.pdf -
Effect of different cooking methods on vegetable oxalate content. J Agric Food Chem. 2005 Apr 20;53(8):3027-30. doi: 10.1021/jf048128d. PMID: 15826055.; Chai W, Liebman M. ;
https://pubmed.ncbi.nlm.nih.gov/15826055/ -
Is There Such a Thing as "Anti-Nutrients"? A Narrative Review of Perceived Problematic Plant Compounds. Nutrients. 2020 Sep 24;12(10):2929. doi: 10.3390/nu12102929. PMID: 32987890; PMCID: PMC7600777.; Petroski W, Minich DM.;
https://pubmed.ncbi.nlm.nih.gov/32987890/ -
Calcium oxalate stone - Causes, prevention, treatment | National Kidney Foundation;
https://www.kidney.org/kidney-topics/calcium-oxalate-stones -
Whole Diet Approach to Calcium Oxalate Kidney Stone Prevention, Journal of Renal Nutrition, Volume 32, Issue 1, 2022, Pages e11-e17, SSN 1051-2276, https://doi.org/10.1053/j.jrn.2021.10.005.; Betz, Melanie.;
https://pubmed.ncbi.nlm.nih.gov/34980366/ -
Vitamin C-Sources, Physiological Role, Kinetics, Deficiency, Use, Toxicity, and Determination. Nutrients. 2021 Feb 13;13(2):615. doi: 10.3390/nu13020615. PMID: 33668681; PMCID: PMC7918462.; Doseděl M, Jirkovský E, Macáková K, Krčmová LK, Javorská L, Pourová J, Mercolini L, Remião F, Nováková L, Mladěnka P, On Behalf Of The Oemonom. ;
https://pubmed.ncbi.nlm.nih.gov/33668681/ -
The Safe and Effective Use of Plant-Based Diets with Guidelines for Health Professionals. Nutrients. 2021 Nov 19;13(11):4144. doi: 10.3390/nu13114144. PMID: 34836399; PMCID: PMC8623061; Craig WJ, Mangels AR, Fresán U, Marsh K, Miles FL, Saunders AV, Haddad EH, Heskey CE, Johnston P, Larson-Meyer E, Orlich M. ;
https://pubmed.ncbi.nlm.nih.gov/34836399/











