Everything to Know About the Diverticulitis Diet
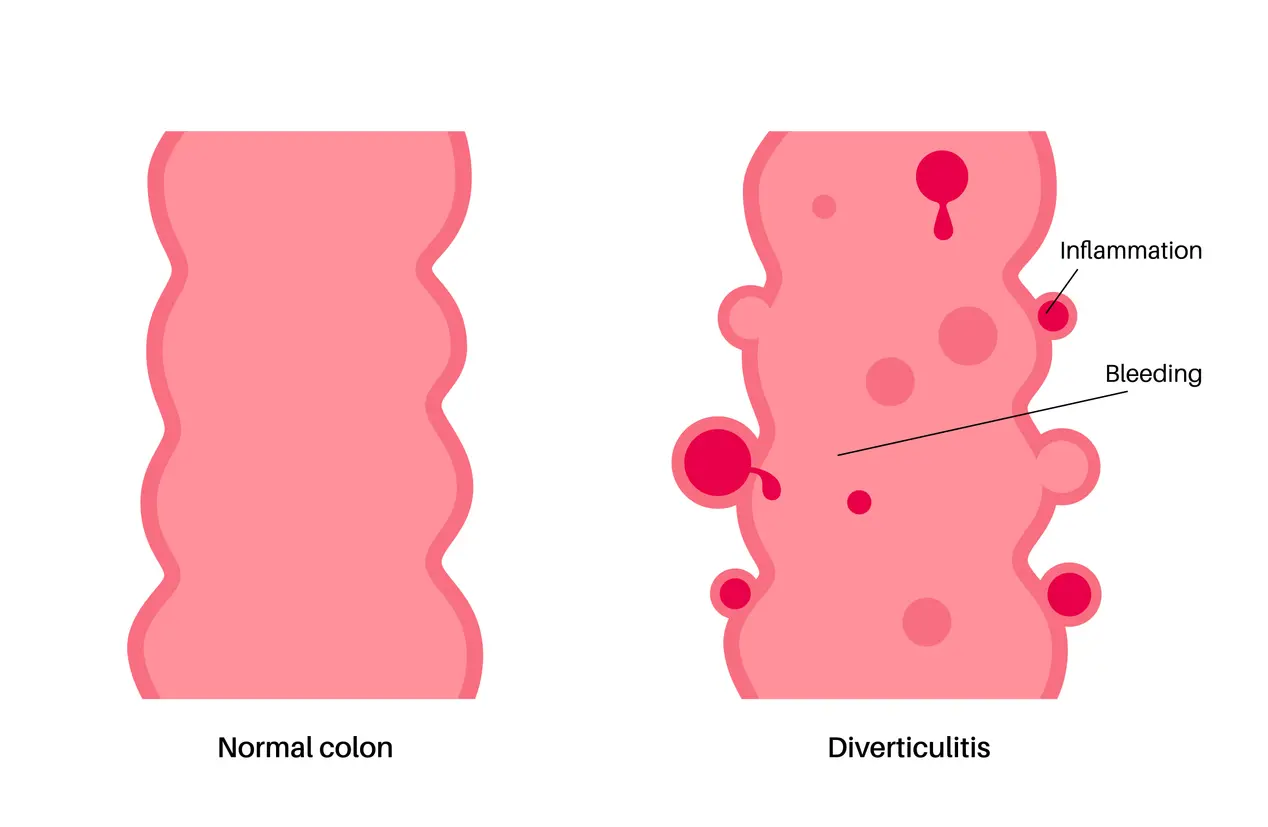
Diverticulitis is a gastrointestinal disorder that occurs when diverticula, which are small pouches in the wall of the colon, become infected or inflamed. The condition is very prevalent, especially in adults over 40 years old [1] Alexander T Hawkins, Paul E Wise, Tiffany Chan et al. Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862 , and may cause symptoms like pain in the abdomen, bloating, nausea, and changes in bowel movements.
Diet is a significant factor in both easing flare-ups and preventing recurrences. When there is an active flare, some foods can rest the digestive tract and minimize discomfort. As symptoms improve, a switch to a low-fiber diet, and then eventually to a well-balanced, high-fiber plan, can aid in healing and long-term colon health.
In this article, we will cover what to eat during a flare-up, how to safely reintroduce foods as you recover, and which eating habits can help reduce the risk of future complications.
Related: What To Eat When You Have Diarrhea And What To Avoid
What Is Diverticulitis?
Diverticulitis is an inflammatory condition that affects small bulging pouches, called diverticula, which form in the lining of the colon. These pouches are common in adults older than 40, and the occurrence of diverticula without inflammation is referred to as diverticulosis. Diverticulitis develops when one or more of these pouches become inflamed or infected. [2] NIH Overview: Diverticular disease and diverticulitis
Common Symptoms
- Persistent abdominal pain, often in the lower left side
- Bloating or abdominal tenderness
- Nausea or vomiting
- Fever and chills
- Constipation or diarrhea
- In more severe cases, complications can occur, such as abscesses, perforations, or intestinal blockages.
What Causes It
Diverticulitis typically develops when stool, bacteria, or undigested food become trapped in a diverticulum, leading to inflammation or infection. Other factors that may increase risk include aging, a low-fiber diet, a sedentary lifestyle, obesity, and smoking. [1] Alexander T Hawkins, Paul E Wise, Tiffany Chan et al. Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862
Why Diet Matters for Diverticulitis
Diet plays a central role in both managing diverticulitis flare-ups and preventing future episodes. Adjusting what you eat can help reduce inflammation during acute symptoms, support healing during recovery, and lower the risk of recurrence long term.
1. During Flare-Ups
When the pouches in the colon are inflammed, your gut needs time to rest. Following a clear liquid diet is typically suggested for 1-3 days to reduce digestive strain. This diet allows the colon to heal while preventing further irritation. [3] Anne F Peery, Aasma Shaukat, Lisa L Strate AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review, Gastroenterology. 2020 Dec 3;160(3):906–911.e1. doi: 10.1053/j.gastro.2020.09.059
2. Transitioning to Recovery
Once symptoms improve, a low-fiber diet is introduced for several days to transition back to a normal diet. Introducing soft, easily digestible foods like white rice, plain yogurt, eggs, and skinless potatoes help the gut recover without causing additional stress. [4] Camilla Dahl, Megan Crichton, Julie Jenkins, Romina Nucera et al. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review: 2018 Jan 27;10(2):137. doi: 10.3390/nu10020137
3. Long-Term Prevention
After full recovery, a high-fiber diet is key to reducing the risk of future flare-ups. Dietary fiber softens stool and improves bowel regularity, lowering the pressure inside the colon and helping prevent diverticula from becoming inflamed. [5] Barbara Gordon, RDN, LD and Esther Ellis, MS, RDN, LDN Diverticulitis
Diverticulitis Flare-Up Diet (Clear Liquid Phase)
When there is an active diverticulitis flare, the goal is to rest the colon and try to decrease inflammation. A clear liquid diet is usually prescribed for a brief time, usually 1 to 3 days, until the symptoms get better. This strategy reduces digestive effort while healing with hydration and electrolyte balance. [3] Anne F Peery, Aasma Shaukat, Lisa L Strate AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review, Gastroenterology. 2020 Dec 3;160(3):906–911.e1. doi: 10.1053/j.gastro.2020.09.059
Recommended Clear Liquids
These options are gentle on the digestive system and provide hydration and some energy:
- Clear broths (chicken, beef, or vegetable)
- Apple juice or other pulp-free fruit juices
- Plain gelatin
- Ice pops made without dairy or fruit pulp
- Water and electrolyte-replacement drinks
- Decaffeinated tea or black coffee (without cream)
Note: A clear liquid diet is not meant to be long-term. It should only be followed until symptoms improve or as directed by your healthcare provider. [6] NIH Therapeutic Diets for the Management of Gastrointestinal Conditions and Pre- and Postoperative Care
Low-Fiber Diet for Early Recovery
As acute inflammation settles and symptoms start to get better, the next phase is to follow a low-fiber diet. The goal in this phase is to add soft, easily tolerated foods that are still gentle to the colon. This phase usually lasts for a few days to a week, depending on symptom severity and your doctor's recommendation. [4] Camilla Dahl, Megan Crichton, Julie Jenkins, Romina Nucera et al. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review: 2018 Jan 27;10(2):137. doi: 10.3390/nu10020137
Examples of Low-Fiber Foods
- White rice
- Refined pasta or bread
- Cooked vegetables such as carrots, zucchini, or green beans (skins removed)
- Skinless potatoes
- Plain yogurt or kefir
- Soft, well-cooked eggs
- White bread or refined grain products
- Tender, skinless poultry or fish
During the transition stage, avoid high-fiber foods like raw vegetables, seeds, nuts, and whole grains, which can irritate the colon and slow recovery. [4] Camilla Dahl, Megan Crichton, Julie Jenkins, Romina Nucera et al. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review: 2018 Jan 27;10(2):137. doi: 10.3390/nu10020137
Sample Diverticulitis Meal Plan
- Liquid Phase: Clear broth + apple juice (no pulp) + plain gelatin + water or electrolyte drink
- Low-Fiber Phase: Scrambled eggs + white toast (no butter) + steamed carrots + plain yogurt
- High-Fiber Phase: Whole grain bread or crackers + lentil soup + salad with leafy greens + pear (with skin)
Staying Hydrated
Make sure to drink lots of water during the day, especially as you increase your fiber consumption. This can help prevent constipation and supports gut motility. [1] Alexander T Hawkins, Paul E Wise, Tiffany Chan et al. Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862
Gradual Progression Through Phases
Transition from each stage based on symptom improvement and your doctor’s advice. Avoid rushing into high-fiber foods too early, which can aggravate symptoms during recovery. [4] Camilla Dahl, Megan Crichton, Julie Jenkins, Romina Nucera et al. Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review: 2018 Jan 27;10(2):137. doi: 10.3390/nu10020137
Tips for Preventing Future Flare-Ups
Long-term management of diverticulitis goes beyond adding fiber to your diet. A consistent, healthy lifestyle can reduce the risk of recurrence and support digestive health.
- Stay well-hydrated: Aim for 8 to 10 cups of fluid daily, especially when consuming high-fiber foods. [1] Alexander T Hawkins, Paul E Wise, Tiffany Chan et al. Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862
- Regular exercise: Physical activity promotes healthy digestion and helps prevent constipation. [5] Barbara Gordon, RDN, LD and Esther Ellis, MS, RDN, LDN Diverticulitis
- Avoid frequent constipation: Straining increases pressure in the colon and may contribute to diverticular complications. Fiber, fluids, and movement all help reduce risk. [5] Barbara Gordon, RDN, LD and Esther Ellis, MS, RDN, LDN Diverticulitis
- Limit red and processed meats: Diets high in red meat have been associated with a higher risk of diverticulitis in some studies. [7] Diverticular Disease
- Introduce fiber slowly: Increase fiber intake over 1 to 2 weeks to give your gut time to adjust and avoid discomfort. [1] Alexander T Hawkins, Paul E Wise, Tiffany Chan et al. Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862
When to See a Doctor
While making changes to your diet can help manage diverticulitis, specific symptoms require medical attention. Contact your healthcare provider if you experience:
- Severe or worsening abdominal pain
- Persistent fever or chills
- Vomiting or an inability to keep fluids down
- Blood in your stool or rectal bleeding
- Symptoms that do not improve after a few days on a liquid or low-fiber diet
Early assessment and treatment are essential to prevent complications such as abscesses, fistulas, or bowel obstruction. [2] NIH Overview: Diverticular disease and diverticulitis
Conclusion
Planning your diverticulitis diet can relieve symptoms during an attack, aid in healing during recovery, and help prevent attacks in the future. From gut rest with clear liquids to the gradual return of fiber-containing foods, each phase serves to manage the condition. Combining dietary approaches with fluid intake, activity, and follow-up with a physician can ensure long-term digestive well-being.
Always follow your doctor’s guidance and adjust your diet based on your individual response and needs.
Was this article helpful?
-
Diverticulitis – An Update from the Age Old Paradigm: 2020 Jul 18;57(10):100862. doi: 10.1016/j.cpsurg.2020.100862; Alexander T Hawkins, Paul E Wise, Tiffany Chan et al.;
https://pmc.ncbi.nlm.nih.gov/articles/PMC7575828/ -
Overview: Diverticular disease and diverticulitis; NIH;
https://www.ncbi.nlm.nih.gov/books/NBK507004/ -
AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review, Gastroenterology. 2020 Dec 3;160(3):906–911.e1. doi: 10.1053/j.gastro.2020.09.059; Anne F Peery, Aasma Shaukat, Lisa L Strate ;
https://pmc.ncbi.nlm.nih.gov/articles/PMC7878331/ -
Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review: 2018 Jan 27;10(2):137. doi: 10.3390/nu10020137; Camilla Dahl, Megan Crichton, Julie Jenkins, Romina Nucera et al.;
https://pmc.ncbi.nlm.nih.gov/articles/PMC5852713/ -
Diverticulitis; Barbara Gordon, RDN, LD and Esther Ellis, MS, RDN, LDN;
https://www.eatright.org/health/health-conditions/digestive-and-gastrointestinal/diverticulitis -
Therapeutic Diets for the Management of Gastrointestinal Conditions and Pre- and Postoperative Care; NIH;
https://www.ncbi.nlm.nih.gov/books/NBK538500/ -
Diverticular Disease;
https://nutritionguide.pcrm.org/nutritionguide/view/Nutrition_Guide_for_Clinicians/1342046/all/Diverticular_Disease